Introduction
Looking after your teeth and mouth is important for your overall health. Healthy teeth and gums not only make it easier to enjoy your favorite foods but also prevent various dental problems. This guide will cover everything from preventing tooth decay to finding affordable dental services.
Summary
1. The Fight Against Tooth Decay
3. Mastering Oral Hygiene Techniques
6. Recognizing and Preventing Oral Cancer
7. Finding Affordable Dental Care
8. The Importance of Regular Checkups
9. Adopting Healthy Lifestyle Habits
1. The Fight Against Tooth Decay

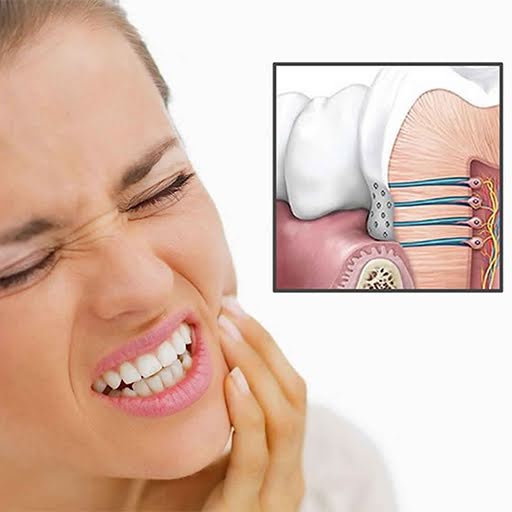
Tooth decay is a common issue that occurs when plaque, a thin film of bacteria, builds up on your teeth. The bacteria in plaque produce acids that can damage the enamel, the hard outer coating of your teeth, leading to cavities.
Preventing Tooth Decay:
- Daily Brushing and Flossing: Brush your teeth twice a day with fluoride toothpaste and floss daily to get rid of plaque and food stuck between your teeth.
- Professional Dental Care: Regular dentist visits are important. If you have a higher risk of tooth decay, such as from dry mouth, your dentist might give you fluoride treatments.
- Healthy Diet: Avoid sugary and acidic foods that can cause tooth decay. Drinking lots of water and eating a balanced diet also help keep your teeth healthy.
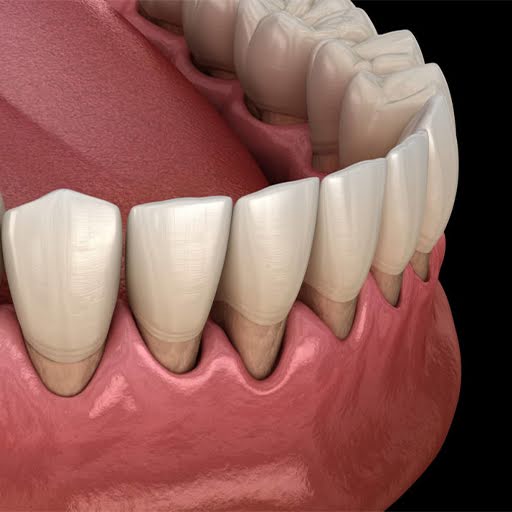
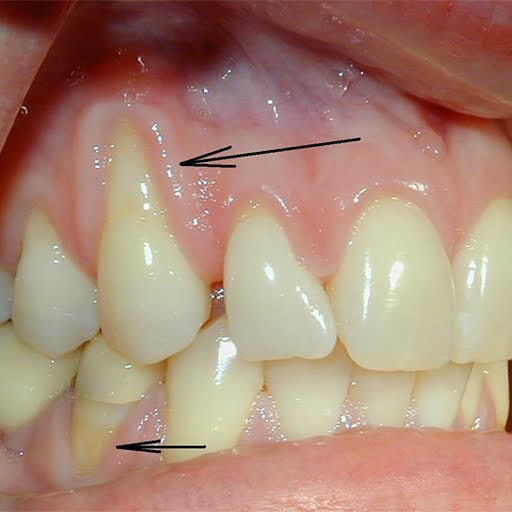
2. Understanding Gum Disease

Gum disease, also known as periodontal disease, starts when plaque builds up along and under the gum line. If left untreated, it can cause serious problems.
Preventing Gum Disease:
- Good Oral Hygiene: Brush your teeth with fluoride toothpaste and floss daily.
- Regular Dental Checkups: Visit your dentist routinely for cleanings and checkups. Inform your dentist about any medical conditions or medications you take.
- Healthy Lifestyle Choices: Eat a well-balanced diet and quit smoking, as smoking increases the risk of gum disease.
3. Mastering Oral Hygiene Techniques

Proper brushing and flossing techniques are vital for maintaining healthy teeth and gums.
Effective Brushing:
- Choose the Right Brush: Use a soft-bristle toothbrush and replace it every 3 to 4 months.
- Gentle Motions: Brush gently on all sides of your teeth using small circular motions and short back-and-forth strokes. Pay special attention to the gum line.
- Tongue Care: Lightly brush your tongue or use a tongue scraper to remove bacteria and freshen your breath.
Effective Flossing:
- Daily Flossing: Clean between your teeth with dental floss, pre-threaded flossers, or water flossers to remove plaque and food particles.
- Proper Technique: Slide the floss gently between your teeth and curve it around each tooth, moving it up and down to clean the sides of the teeth.
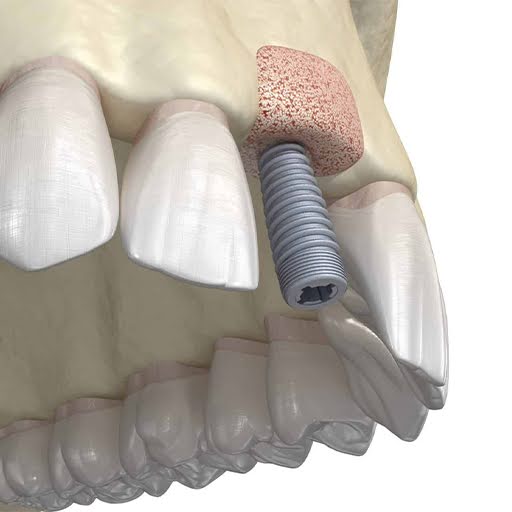
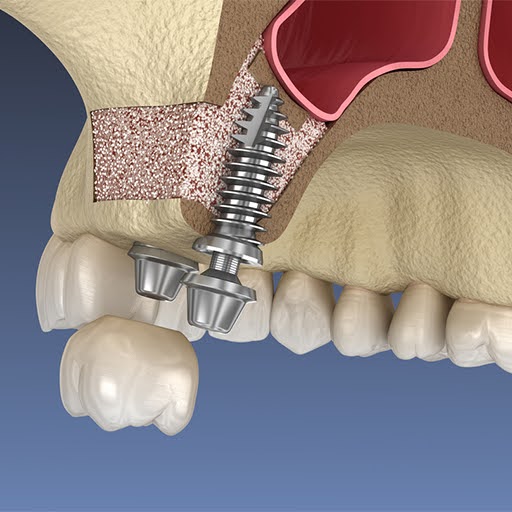
4. Adapting to Dentures

For those who have lost teeth due to gum disease or other issues, dentures can be a good solution. However, they require proper care and adjustment.
Caring for Dentures:
- Cleaning: Brush dentures daily with a denture-care product and soak them in water or a denture-cleaning solution overnight.
- Adjustment Period: Initially, dentures may feel strange. Follow your dentist’s instructions to ensure a proper fit and adjust over time.
5. Managing Dry Mouth

Dry mouth happens when there isn’t enough saliva to keep your mouth moist. It can lead to various oral health problems.
Relieving Dry Mouth:
- Stay Hydrated: Sip water or sugarless drinks throughout the day.
- Avoid Irritants: Stay away from tobacco, alcohol, caffeine, and acidic or spicy foods.
- Stimulate Saliva Production: Chew sugarless gum or suck on sugarless candy. Your dentist may also recommend artificial saliva products.
6. Recognizing and Preventing Oral Cancer

Oral cancer can develop in any part of the mouth or throat and is more common in people over 40.
Preventing Oral Cancer:
- Avoid Tobacco and Limit Alcohol: Refrain from using tobacco products and drink alcohol in moderation.
- Regular Dental Checkups: Dental visits are an opportunity for your dentist to check for signs of oral cancer. Early detection improves treatment outcomes.
- Protect Your Lips: Use lip balm with sunscreen to protect against sun damage.
7. Finding Affordable Dental Care

Dental care can be expensive, but there are options to find affordable services.
Low-Cost Dental Care Options:
- Dental Schools: Many dental schools offer low-cost clinics where students treat patients under professional supervision.
- Community Health Centers: These centers often provide dental services based on your income.
- United Way and Other Organizations: Local United Way chapters can direct you to free or reduced-cost dental services.
8. The Importance of Regular Checkups

Regular dental checkups are essential for maintaining oral health and catching problems early.
Benefits of Regular Checkups:
- Early Detection: Your dentist can identify issues like cavities, gum disease, and oral cancer early when they are easier to treat.
- Professional Cleaning: Dental cleanings remove plaque and tartar buildup that regular brushing and flossing miss.
- Personalized Advice: Your dentist can provide tailored advice on improving your oral hygiene routine and addressing specific concerns.
9. Adopting Healthy Lifestyle Habits

Your lifestyle choices play a significant role in your oral health.
Healthy Habits:
- Balanced Diet: Eat a mix of foods like fruits, vegetables, lean proteins, and whole grains.
- Avoid Tobacco: Smoking and using other tobacco products can lead to gum disease, tooth loss, and oral cancer.
- Stay Hydrated: Drinking water helps wash away food particles and keeps your mouth hydrated, which is essential for preventing dry mouth and tooth decay.
FAQs
Q.1. How often should I brush and floss?
A.1. Brush twice a day and floss once daily to maintain optimal oral health.
Q.2. What should I do if my gums bleed when I brush or floss?
A.2. Consult your dentist if you experience bleeding gums, as this can be a sign of gum disease..
Q.3. How can I keep my dentures clean?
A.3. Brush them daily with a denture-care product and soak them overnight in a denture-cleaning solution.
Q.4. What are the signs of oral cancer?
A.4. Early signs include sores that do not heal, lumps, or white or red patches in the mouth. Regular dental checkups are important for finding problems early.
Q.5. Are electric toothbrushes better than manual ones?
A.5. Electric toothbrushes can be more effective, especially for people with limited hand mobility, but proper technique is crucial regardless of the type of toothbrush.
Conclusion
Taking care of your teeth and mouth is essential for your overall health and well-being. By following good oral hygiene practices, making healthy lifestyle choices, and seeking regular dental care, you can maintain a bright, healthy smile for life.
For personalized help or to schedule a consultation, contact our team at (267) 908-4867 or visit our website at https://premierperiodonticspa.com/. Your smile is our top priority. We’re here to provide the guidance and support you need for a comfortable dental experience. Trust us to care for your oral health and help you achieve a bright and healthy smile. We look forward to working with you.